ARTICLE AD BOX
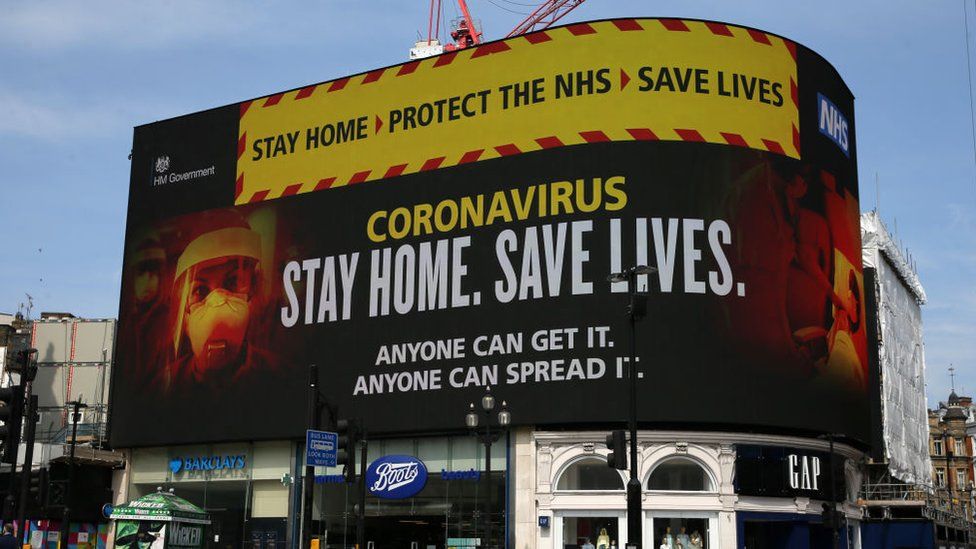 Image source, Getty Images
Image source, Getty Images
Huge signs showing health advice adorned the large screens at Piccadilly Circus in London in April 2020
People with underlying conditions who called the 111 Covid phoneline early in the pandemic were not always properly assessed or seen by a doctor, the health safety watchdog has found.
The Healthcare Safety Investigation Branch (HSIB) heard from the families of four people who called NHS 111 and later died because of Covid-19.
There was huge demand on the system in March 2020, caused by the virus.
NHS England said there were many unknowns at the start of the pandemic.
An NHS spokesperson said: "111 played a vital role in managing the response to the pandemic and despite unprecedented demand, answering over two million calls in March 2020 alone, both 111 and the coronavirus response service referred more than half a million patients for further clinical assessments - including in face-to-face settings."
"Call handlers followed guidance set out by Public Health England which was regularly updated as the understanding of Covid-19 improved, and the NHS has captured learning throughout the last two years to contribute to the response to any future pandemics."
The HSIB report said lessons should be learned for the future and advice should be clearer.
It looked at issues getting through to NHS 111, and the advice provided to four people with Covid-19 between March and June 2020.
They all had other major health issues, yet some did not receive advice directly from a doctor or see one face to face, despite their condition worsening.
The report found that aspects of the telephone triage system "did not function as intended".
Four people who called 111
- Vincenzo, 62, who had diabetes, started to feel unwell with Covid-like symptoms in March 2020. He and his family called NHS 111 many times; some calls were not answered. When he did get through, he was advised to self-care at home. His family called 999 on 26 March when his condition deteriorated. He died in hospital on 1 April 2020
- Ali, 66, had diabetes and hypertension (high blood pressure). He and his wife made three calls to NHS 111 over three days in April 2020. A doctor called back to discuss his symptoms and he was advised to stay at home. He collapsed and his wife called 999 but Ali was declared dead by paramedics when they arrived. Ali died from acute respiratory symptoms, which led to a cardiac arrest, because of Covid-19
- Patrick, 60, had multiple sclerosis and worked on a Covid ward at his hospital trust. He made three calls to NHS 111 over a few days in April and was advised to remain at home. The next day he called an ambulance after contacting a colleague for advice. He was taken to hospital and put on a ventilator. He died eight days later on 19 April 2020
- Dr C, 45, had type 2 diabetes. He called NHS 111 three times over two days in March 2020 with Covid symptoms and received a call back from a doctor. He was prescribed an inhaler and antibiotics. His partner called 999 a day later as his condition had worsened. He was taken to hospital and died 16 days later on 3 April 2020
At that time of these calls, anyone who dialled the NHS 111 phoneline was either managed through NHS 111 or - if they had Covid-like symptoms - through the Covid Response Service.
But the report found that the callers were often only transferred to a doctor, or called back by one, when they were so ill that they had stopped doing all of their usual daily activities.
Image source, Getty Images
And Covid-related calls which went through to the core NHS 111 service were not always redirected to the Covid service, and some were never recorded.
The HSIB says the knock-on effect of messaging to stay at home in the early months of the pandemic "may have impacted on patients' willingness to seek medical advice from elsewhere (such as their GP)", even if their condition got worse.
Clear advice
Amber Sargent, national investigator at HSIB, said systems had to be put in place at short notice and there were many unknowns when the NHS started tackling a brand new coronavirus in 2020.
She said: "Anyone may need to access NHS 111 or other telephone triage when there is an emerging healthcare crisis.
"It is critical that services can be stood up within a short timeframe and that communication of messages and advice to the public is as clear as possible to help them get the crucial care and treatment they may need."
In future, advice on symptoms to look out for, where to go for medical help and what to do if their condition worsens should be clearly provided, the report said.
To improve the safety of the NHS 111 service in another pandemic, the report recommends that the language used by health advisers does not deter seriously unwell people from calling back or seeking help.
It also notes the benefits of face-to-face assessment for callers with other health conditions faced with a new virus.
The HSIB carries out investigations of patient safety concerns in NHS-funded care in England.
It noted that the UK Health Security Agency had taken some steps to try to improve safety.
Related Internet Links
The BBC is not responsible for the content of external sites.

 2 years ago
27
2 years ago
27








 English (US)
English (US)