ARTICLE AD BOX
9 hours ago
By Hannah Ritchie, BBC News, Sydney

 Heidi Metcalf
Heidi Metcalf
A recent government survey found that two thirds of women, like Heidi Metcalf, have encountered gender bias or discrimination in Australian healthcare
There’s a memory, or more specifically a moment, that came to define Heidi Metcalf’s second birth.
It wasn’t saying goodbye to her husband and newborn before being wheeled into an operating theatre, or the heart attack she thought she was having as she lay there on the table.
It was when a male obstetrician “ripped the placenta” out of her body, without word or warning.
A nurse, Ms Metcalf knows the intervention - while immensely painful - was necessary. She couldn't push it out naturally, which was causing potentially fatal bleeding.
But she hadn’t “seen or met this man before”, and she can’t get past the fact that her consent, during one of the most traumatic experiences of her life, “meant so little”.
“It felt like a violation - I needed to feel involved in what was happening to my body, and not just like a bystander.”
Ms Metcalf is one of thousands of Australian women who have come forward to tell their stories, after the federal government assembled a team of experts to tackle what it calls “medical misogyny”.
So far, they have uncovered that a staggering two-thirds of females nationwide have encountered gender bias or discrimination in healthcare.
And many say it is taking place when they're at their most vulnerable, such as during intimate examinations, or like Ms Metcalf, while in labour. Others report having their pain dismissed or dangerously misdiagnosed.
The BBC spoke to six women for this piece. They shared experiences of being called “anxious”, “pushy” or even “hysterical” while seeking treatment for a range of debilitating symptoms.
They also said they felt that the men in their lives seemed to consistently have their pain taken more seriously.
'I just don't feel safe'
Nadiah Akbar was once told by a doctor in Singapore that the extreme fatigue she was experiencing was due to the “stress” of being a busy mother. Tests would later show it was thyroid cancer.

 Nadiah Akbar
Nadiah Akbar
Nadiah Akbar says she has been misdiagnosed repeatedly - often having her symptoms dismissed as stress releated
Years later, in remission and having migrated to Australia, staff at a Melbourne hospital failed to diagnose a cartilage tear in her hip socket and a slip disk in her back.
Instead, they suggested the crippling pain could be linked to “depression” or being “overtired”. It led to Ms Akbar paying for two costly MRI scans out of pocket to be taken seriously.
“‘Oh, it’s nothing.’ I’ve heard that statement so many times... It’s really disheartening as a human being to keep hearing that,” she says.
“It takes a lot of energy for you to keep advocating for yourself, and that’s the part that’s worrying - a lot of people just stop.”
Laura - who asked to have her name changed - is close to that point, after years of having symtoms of what would eventually be confirmed as a traumatic brain injury dismissed.
“I don’t get healthcare without my partner with me, that’s a blanket rule,” she says, explaining that she feels her concerns are taken “more seriously” when voiced by a man.
“I just don't feel safe, engaging with the system, because when you're young and you're told over and over that something is all in your head, it's easy to believe it.”
Like so many others across the country, both women say they’re coming forward to share their experiences to seize on this moment of promised change.
Assistant health minister Ged Kearney - who chairs the national council tasked with examining these issues - says that their stories, along with those of countless others facing additional disadvantage in First Nations, LGBTQ+, and migrant communities will guide its work.
Her team's remit is vast and broad areas of focus have already emerged.
But untangling gender inequity in medicine is no small task, and Australia’s attempts could have far-reaching implications as other nations eye reforms.

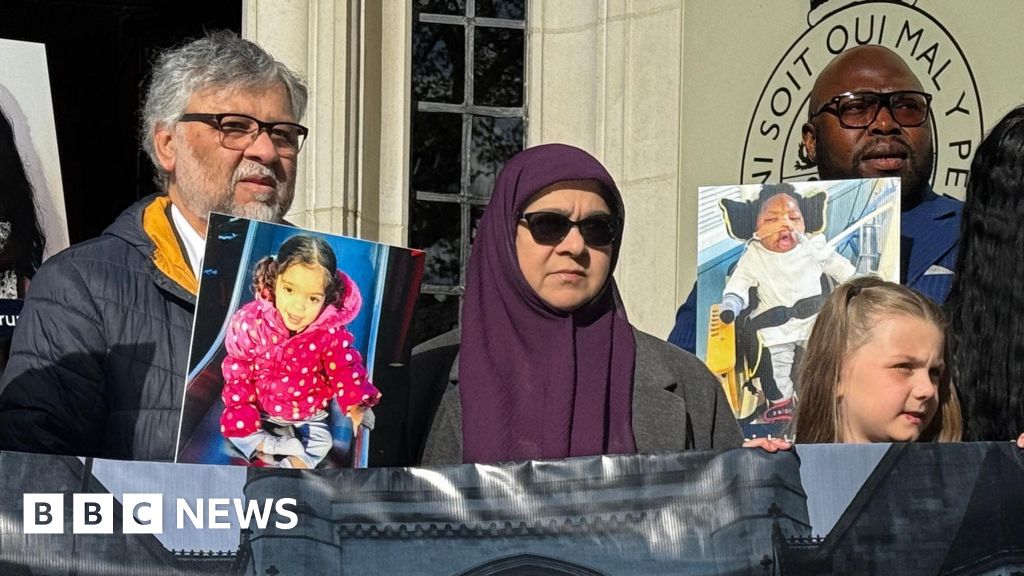
 Ged Kearney
Ged Kearney
Assistant health minister Ged Kearney with her daughter and granddaughter
'A one-size-fits-all approach'
The problem is not that “all healthcare professionals have some set agenda against women”, Ms Kearny says.
Rather it's that bias is woven into the fabric of modern medicine because for centuries it was “delivered by and designed for” men.
Women’s health - by contrast – was often rooted in myth and pernicious gender stereotypes.
“Hysteria”, a now-defunct medical term, was a catch-all diagnosis for females presenting with an array of symptoms, meaning their pain was attributed to emotional causes, rather than biological ones.
But today, some women say they continue to feel gaslit - disbelieved and patronised - in medical settings.
And a lack of diversity in medical research compounds the issue.
More than 70% of participants in early-stage clinical trials globally are still white men, while male cells and animals are used as standard in the lab, according to Professor Robyn Norton, a public health expert.
The results are then applied to women, intersex, trans and gender-diverse people, causing issues when it comes to their treatment, diagnosis and how their symptoms are understood, Prof Norton says.
She describes it as a “one-size-fits-all, male-centric” approach to healthcare that has created huge knowledge gaps.
One analysis carried out in 2019 by the Novo Nordisk Foundation Center for Protein Research - which used data from the entire Danish population - found that, across 770 diseases they studied, women were diagnosed later than men, with an average lag time of four years.
In Australia, research from the University of Sydney in 2018 found that females admitted to hospital for serious heart attack were half as likely as men to get proper treatment and that they died at twice the rate six months after discharge.
Scientists have warned that another roadblock is the chronic underinvestment in women-specific health issues.
Endometriosis is pointed to as a key example. Despite impacting roughly 10% of reproductive-age women and girls globally, there is no cure, and it takes seven years on average for patients to be diagnosed.
One recent study found that 89% of Australian women were still being advised by health professionals that pregnancy would fix their symptoms - despite growing evidence it's a medical fallacy.
Such disparities are being recognised and investigated globally, experts say - with countries comparing notes on what might be the best approach.
The UK, for one, recently announced measures aimed at closing the “gender health gap” in its system. And in the US, the federal government has launched an initiative to improve funding and research into women’s health, led by First Lady Jill Biden.

 Bonney Corbin/Australian Women's Health Alliance
Bonney Corbin/Australian Women's Health Alliance
Bonney Corbin has spent her career trying to make Australian healthcare more equitable
Ms Kearny says Australia is already making inroads.
In the past 12 months, her government has opened 22 endometriosis and pelvic pain clinics aimed at improving care and diagnosis.
The nation's drug regulator has removed restrictions on prescribing and dispensing medical abortion pills to increase universal access to reproductive healthcare.
And researchers will soon be able to examine how key diseases are experienced in female, intersex and gender diverse populations at a new centre Prof Norton is leading.
She’s optimistic her team’s work could “catalyse the kind of change in Australia that could see it become a leader in this space”.
There’s also been some investment in women’s health in the latest national budget. Almost A$100m ($66m; £52m) has been set aside for things like reducing the out-of-pocket costs associated with gynaecological conditions, as well as studies into menopause, pregnancy loss and fertility. All are issues which have been historically under-funded.
But while advocates like Bonney Corbin – the chair of Australia’s Women’s Health Alliance who also sits on the council - have welcomed the cash injection, they say it doesn’t go far enough and that state governments should step up too.
“A gender lens on healthcare is more than funding things related to breasts and uteruses. We need to look at women’s bodies on the whole,” she explains.
In the coming months, Ms Kearney's advisory body will release its first set of major reform recommendations.
She says it has no intention of putting forward “tick-box” measures that tinker around the edges.
Instead, she says the long-term goal is to create a blueprint to “build a healthcare system that actually works for everyone”.
Whether the advice will lead to lasting change remains an open question despite the assistant health minister’s participation at this point, Ms Corbin says.
If it doesn’t though, she hints that there could be public backlash.
“We’ve mobilised a whole lot of women in this process – now we need action.”

 9 months ago
43
9 months ago
43







 English (US) ·
English (US) ·