ARTICLE AD BOX

Dr Jasna Macanovic was sacked after she complained about the kidney dialysis practice
By Michael Buchanan
BBC News
A group of doctors offered a controversial medical technique which allegedly put kidney patients' health at risk.
At least 20 patients at Queen Alexandra Hospital (QA) in Portsmouth have been using the procedure, which is not recommended in UK guidelines.
A consultant was wrongly sacked from the hospital in 2018 after objecting to the practice.
The hospital trust said the safety and care of its patients was its priority.
Jasna Macanovic, who worked at the QA for 17 years, had raised concerns about the way the trust was allowing some staff to deliver the dialysis technique - known as buttonholing.
"I don't think they're fit to practise medicine," Dr Macanovic told the BBC.
All patients using a dialysis machine - which cleans their blood because their kidneys can no longer do this - need to have a special strengthened blood vessel made for them, to connect to the machine. Usually this is a fistula, made by joining an artery with a vein, but for a small number of patients whose veins are fragile, a piece of plastic tubing called an arterio-venous graft is used instead.
Needles connect the graft to the machine, and are normally inserted into different places on the graft each time - a technique known as rope-laddering.
Buttonholing, on the other hand, involves putting needles into the same hole each time. This is safe for those with fistulas, but for those using grafts, it "has always been avoided... due to the risk of infection and graft degradation", according to the UK Kidney Association guidelines which are used throughout the NHS. It says only rope-laddering is recommended for grafts.
International guidelines, and the grafts' manufacturer, go further, describing the practice as contraindicated, meaning it may be harmful to patients.
Nonetheless a small team at Portsmouth - including consultants Paul Gibbs and Nick Sangala, as well as nurse Sarah Kattenhorn - championed the procedure.
When Dr Macanovic examined the records of 15 patients using the buttonholing technique at the QA, she found infection rates four times higher than they experienced using the standard technique.
One of the patients featured in Dr Macanovic's audit was Amanda Kelsey, who died in April 2020, aged 50.
Image source, Family handout
Image caption,Amanda Kelsey had suffered kidney problems since birth
Her death certificate gave the cause of death as a stroke, end-stage renal failure and Covid-19. Her husband repeatedly asked the hospital to investigate why her blood pressure had suddenly increased in the months before her death. He says he never got an answer on this, and both he and Dr Macanovic now wonder if it was linked in some way to the complications she had been experiencing with her kidney dialysis.
"We were told it's less aggressive on your skin and on the point of entry into your vein," recalls her husband Mark.
But Mrs Kelsey's medical records, which BBC News has seen, show she suffered a great deal after she started buttonholing. There are repeated references to her graft clotting, with various surgeries to repair it.
"I would say that the buttonhole needling technique destroyed her life, certainly destroyed her health," says Dr Macanovic. "No human body should be put through that trauma."
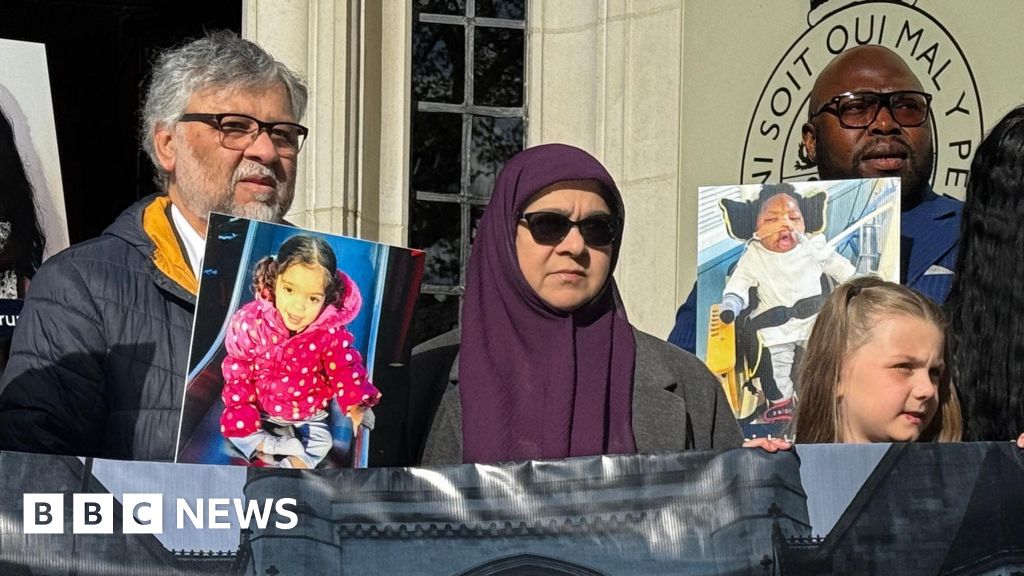
Amanda's husband Mark Kelsey believes buttonholing may have contributed to her death
Dr Macanovic's audit found that Mrs Kelsey's complication rate during buttonholing was almost six times higher than it had been previously, and that in the three years after she started buttonholing, Mrs Kelsey had had at least 18 interventions related to problems with her graft. In the three previous years, when she had been using the standard rope-laddering technique, she had needed just one intervention.
In a statement, the Portsmouth Hospitals University NHS Trust said it wasn't able to comment on Mrs Kelsey's case because of patient confidentiality. It said her death was reviewed by an independent medical examiner, in accordance with the law, and the examiner agreed with the cause of death given by the reporting doctor.
But it did acknowledge that it was "not aware" of any other NHS organisation using buttonholing and that a medical paper evidencing the merits of the technique - that a staff member had publicly promised in 2020 - had not been written or published.
The NHS whistleblowers punished for raising concerns.
Dr Macanovic says she drew her colleagues' attention to several sets of guidelines which outlined the dangers of buttonholing, wrote to the grafts' manufacturers who confirmed that "the buttonhole technique… cannot be used", and reported her colleagues' actions to regulators - the Care Quality Commission (CQC) and the General Medical Council (GMC).
Though the regulators' reviews found there had been problems - for example a CQC inspection found the procedure had been introduced without patients being informed of the dangers of the technique - they didn't stop the procedure. They said safety concerns were taken into account. It also cleared those involved of any misconduct.
An external review commissioned by the trust also found no evidence of direct patient harm, but Dr Macanovic remains unconvinced.
"It's very important for society to understand how weak the regulatory bodies are when it comes to patient safety," she said.
The trust, for its part, said it "does not accept that Dr Macanovic raised evidenced concerns of patient harm" but said her claims had been "fully reviewed by clinicians" at the trust and considered alongside existing reviews and the medical history of each patient.
Dr Macanovic was dismissed in March 2018, but subsequently won £219,000 in compensation for unfair dismissal after taking legal action. The judge in her employment tribunal ruled she had been sacked as a result of her whistleblowing.
Portsmouth Hospitals University NHS Trust told the BBC that while UK vascular access guidelines do not recommend buttonholing, they "do not specifically state that it is contraindicated". It added that other options were always "explored and offered" before this technique was discussed with patients.
The trust added that "Dr Gibbs did not persuade or encourage patients or other clinicians to use the buttonholing AV graft technique" and that he "at all times, properly set out the known advantages and disadvantages of the technique to patients". It added that Dr Gibbs had always "acted properly, in accordance with his obligations as a medical practitioner, and with patient safety in mind".
The trust acknowledged that Dr Sangala and Ms Kattenhorn were supportive of the buttonholing technique and had spoken about it at national and international conferences. It said their 2016 and 2017 conference presentations had also referred to two patient deaths and an excised infected graft, "providing a balanced view of the technique and not misrepresenting the outcomes at these meetings".
"The safety and care of our patients is our priority", said the trust, and "we took the concerns raised by Dr Macanovic in 2016 very seriously". It said it had now stipulated further oversight, including "a comprehensive letter of consent… rigorous surveillance of the patients and recording of complications via our incident recording system".
It added that it "is in full support" of its staff, and is confident in their credibility and ability to practise.

 1 year ago
51
1 year ago
51







 English (US) ·
English (US) ·