ARTICLE AD BOX
Kate Morgan
Communities correspondent, BBC Wales News
 PA
PA
Abortion care provider the British Pregnancy Advisory Service said there was "limited provision" of surgical abortions in Wales after 14 weeks
Wales is the worst part of the UK for providing surgical abortions with many women treated in England, according to a leading healthcare charity.
The British Pregnancy Advisory Service (BPAS) said it was "astonishing" Wales was behind Northern Ireland, where abortion was only decriminalised in 2019.
One south Wales woman said she felt extra trauma and guilt at the thought of being sent away for the procedure - which involves an operation to remove the pregnancy from the womb.
The Welsh government said it accepted improvements needed to be made for mid-trimester (13 to 27 weeks) abortion services, and women should be able to access essential healthcare services closer to home.
In Wales, England and Scotland abortion is allowed up to 24 weeks of pregnancy with the approval of two doctors.
Abortion was decriminalised in Northern Ireland in 2019, and prior to that it was only allowed in very specific circumstances.
Abortion care provider BPAS told BBC Wales that Northern Ireland now offered second trimester surgical abortions beyond 20 weeks, with Scotland offering services up to 20 weeks.
However, in Wales there was "very limited provision after 14 weeks" it said, partly because of a "skills gap" and few doctors.
Sarah, not her real name, found herself unexpectedly pregnant about two years ago.
She was already a mum, and because she had experienced serious post-natal depression in the past, could not face going through with the pregnancy.
Sarah, who is her late 30s, said she did not want a medical abortion because of an earlier miscarriage, but was told she could not have a surgical abortion locally because of an existing medical condition that meant she needed general anaesthetic.
When she was around 16 weeks pregnant, she was offered the procedure in London with her travel and accommodation paid for for two nights.
But she found the whole experience "really stressful".
"There was a bigger sense of guilt, because I was being sent away," Sarah added.
"I was imagining people with placards waving and shouting, I didn't know what hospital it would be.
"Having to leave my two children – who I hadn't left for more than one night – what would we tell them, what would we do? It added a lot of extra stress and trauma."
Sarah decided to continue with the pregnancy, describing it as a "really difficult time" until she was around 28 weeks.
"Emotionally, it was the worst summer of my life," she said.
What is surgical abortion?
- Surgical abortion involves an operation to remove the pregnancy from the womb
- It may be done with local anaesthetic, conscious sedation or general anaesthetic and, according to the NHS, the surgical method can be performed by vacuum or suction aspiration or by dilation and evacuation
- Medical abortions, which involve the use of drugs, accounted for 86% of abortions in Wales and England in 2022
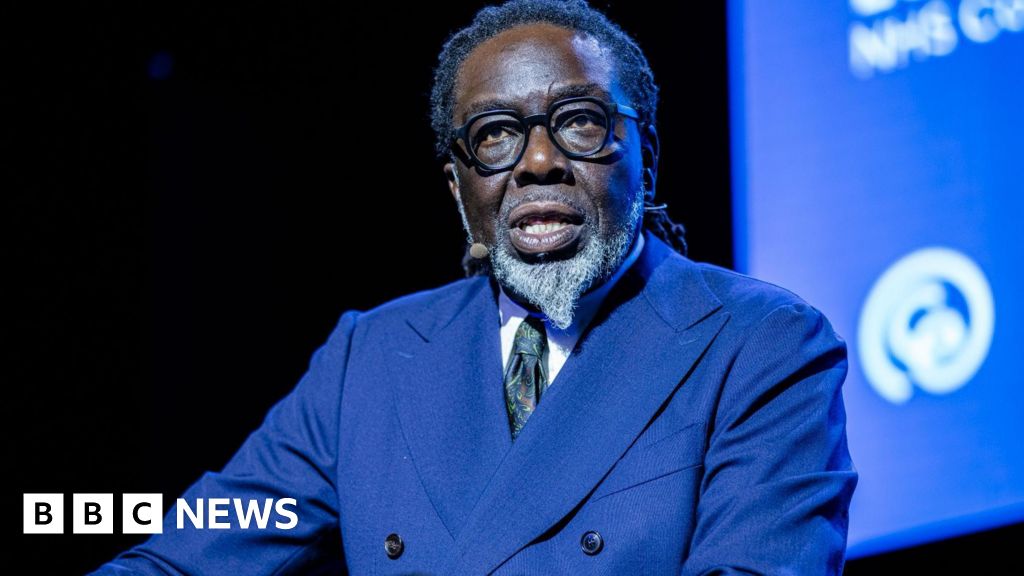
 Rachael Clarke
Rachael Clarke
Rachael Clarke from BPAS said some women may choose to continue pregnancies because of a lack of access to care
Rachael Clarke from BPAS said each year about 175 women travel from Wales to England for care.
"Many of these women don't want to speak out about what they experienced, they don't want to revisit it, and it makes it very easy for people to ignore the quite harrowing experiences," she said.
The head of advocacy added it was often seen as the "easy option" to send women to a different service or country instead of accessing care closer to home.
"A lot of that is down to clinical availability, but also premises," she said.
"If you don't have space in a hospital, if you don't have a theatre, if you don't have a ward where women can go before and after that limits what you're able to provide."
She added that there was a dangerous skills gap with a lack of doctors routinely performing surgical abortions, or procedures also used in mid-trimester miscarriage.
The first women's health plan for Wales, published in December last year, lists abortion as a "fundamental aspect" of women's reproductive healthcare, stating it should be available "locally and without delay for all women" to reduce "complications, distress and cost".
Funding and delivering services for mid-trimester abortion care is listed as a long-term goal, with a timescale of approximately six to 10 years.
Ms Clarke described that timeline as "a kick in the guts".

Plaid Cymru's Sioned Williams raised the issue in the Senedd earlier this year
MS Sioned Williams said the women's health cross-party group had been asking the Welsh government to act since 2018.
"It's important to me that when we say something is a health right, as it states in the new women's health plan, that there's action behind that to make it so, and that people are able to access abortions in a timely way," she said.
The Plaid Cymru MS for South Wales West added she thought this could be easily changed because of the relatively small number of women who require this care.
A spokesperson for the Welsh government accepted that improvements in mid-trimester abortion services need to be made, adding it fully acknowledges that women should be able to access essential healthcare services closer to home.
"We are working with NHS Wales to identify and address the specific barriers to providing surgical abortion services locally and we are exploring what short-term improvements we can make while developing a robust, sustainable service for the future", they added.

 1 day ago
10
1 day ago
10







 English (US) ·
English (US) ·